Asthma treated in mice using offshoot of CAR T-cell cancer therapy


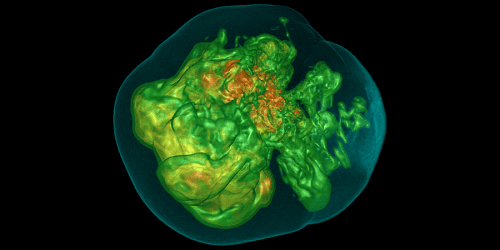
An eosinophil immune cell, which can be involved in asthma
KATERYNA KON/SCIENCE PHOTO LIBRARY/Alamy
It might be possible to effectively cure the most common form of asthma by using genetically engineered cells to kill off the rogue immune cells that trigger asthma attacks, a study in mice suggests.
But making this kind of treatment affordable will be a major challenge, and its risks mean it would probably be given only to those who get life-threatening asthma attacks.
“For most asthma patients, an inhaler is probably enough, however, approximately 250,000 people die from severe asthma annually,” says Min Peng at Tsinghua University in Beijing, China. “[This] could be an option for those patients.”
Asthma is a condition in which the airways swell and narrow, making it difficult to breathe. Asthma attacks can be triggered by factors such as allergies or air pollution.
Most cases of asthma involve a process called the type 2 immune response. This is meant to protect against parasites such as worms but can lead to excess numbers of immune cells called eosinophils. Inhaled steroids can usually damp down this response and reduce symptoms, but people with severe asthma may require regular injections of antibodies designed to reduce the number of eosinophils.
It is possible to genetically modify immune cells known as T cells to kill specific cell types. These modified cells, called CAR T-cells, are mainly used to treat certain cancers but have also been used for the autoimmune condition lupus.
Now, Peng and his colleagues have created CAR T-cells that kill eosinophils. In mice induced to have type 2 asthma, a single dose of these cells prevented symptoms for up to a year, which is as long as the experiment lasted. “In mice, these cells persist in vivo indefinitely,” says Peng.
When used to treat cancers, CAR T-cells can cause potentially deadly side effects, but Peng’s team didn’t see these in the mice, which suggests this form of the treatment is safer. Nor was there any sign of the CAR T-cells turning cancerous. But should this therapy be approved for people with asthma, the team says a “kill switch” should be built into any cells just in case.
However, extracting cells from the body, modifying them and replacing them – as is required to generate CAR T-cells – is extremely expensive. Approved CAR T treatments are priced around $400,000 in the US, and the total costs including all medical care can be much higher.
“For prevalent diseases like asthma, an affordable price is critical for making CAR T-cells accessible to the majority of patients,” says Peng. He hopes it will become possible to turn cells in the body directly into CAR T-cells without extracting them, which would greatly reduce costs.
Topics:
Read the original article here