Bioelectronic patch uses living bacteria to treat psoriasis in mice


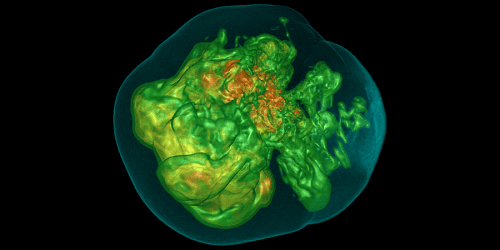
This living bioelectronic device is being used to treat psoriasis in mice
Jiuyun Shi and Bozhi Tian/University of Chicago
A bioelectronic device that incorporates living skin bacteria reduces inflammation and boosts healthy skin regeneration in mice experiencing psoriasis, a chronic autoimmune disease that is characterised by the accelerated growth of skin cells. A future version of the technology might help treat some of the 125 million people worldwide with psoriasis.
“For the mouse model, four days or close to one week should be enough for treatment,” says Bozhi Tian at the University of Chicago, whose team developed the device. “If you’re thinking about the potential clinical application in a human subject then a longer time will be needed – but that can easily be done.”
The device’s top layer has electronic sensors that can measure skin electrical impedance – which is a proxy for tracking skin thickness and dryness – along with body temperature and humidity. The bottom layer consists of a soft hydrogel material that contains living Staphylococcus epidermidis bacteria, a component of the normal human skin microbiome. These bacteria are mixed in with starch and gelatine to mimic a “biofilm” in which bacteria can thrive.
The S. epidermis bacteria naturally produce a metabolite capable of disrupting the overactive growth of the skin cells. Over the course of treatment, this metabolite encouraged normal skin growth. The researchers could keep track of the process by monitoring the change in the skin’s electrical impedance and observing the reduction in clinical symptoms.
Such technology could eventually lead to devices that use the sensor information to continually adjust the therapeutic benefits of the living bacteria, writes Peder Olofsson at the Karolinska Institute in Sweden, in a perspective article exploring the implications of the new technology.
Preliminary work by Tian and his colleagues shows how. Their recent study revealed that a middle layer of the device can be used to deliver electrical stimulation following successful treatment, which kills the S. epidermis bacteria and disinfects the skin. But preliminary, unpublished results suggest that certain levels of electrical stimulation can actually boost the therapeutic activity of the skin bacteria rather than killing them. This suggests that, through careful control of the electrical stimulation, it might be possible to speed up or slow down the rate of treatment to meet the needs of the individual being treated.
“What we’re doing right now is to use electrical stimulation to further modulate the microbial activity,” says Tian. “So you can still keep the cells alive but with an enhanced therapeutic effect.”
Topics:
Read the original article here