Wearable optical device could detect postpartum haemorrhage
A new wearable imaging device that monitors changes in blood flow in a patient’s hands, feet or arms could be used as an early warning system for postpartum haemorrhage – a relatively common complication of childbirth that accounts for over 30% of maternal deaths each year. The laser-based sensor, which has been successfully tested in simulated tissues and in pigs, is now being trialled in healthy human volunteers.
Postpartum haemorrhage is the leading cause of maternal mortality worldwide, and it is currently diagnosed either by simple observation or by monitoring standard vital signs such as heart rate and blood pressure. These techniques often underestimate the severity of blood loss because the body responds to haemorrhage by redirecting blood flow to vital organs and restricting it in peripheral areas such as hands, feet and arms. The result – vasoconstriction in peripheral areas, coupled with normal or near-normal blood flow in the body’s core – means that vital signs can remain unchanged until a lot of blood has been lost. Being able to detect peripheral vasoconstriction in real time would therefore alert clinicians to blood loss earlier, enabling them to begin potentially life-saving treatments.
Measuring blood flow
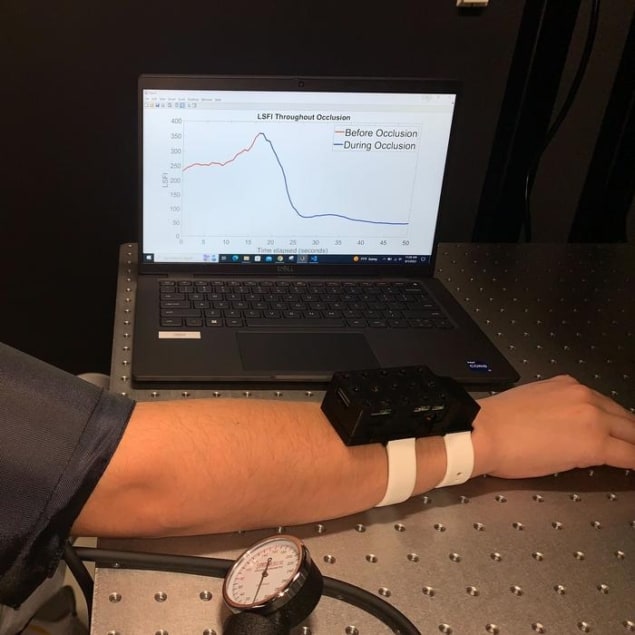
The new device, developed by Christine O’Brien and colleagues at Washington University in St Louis, US, uses a technique called laser speckle contrast imaging to measure blood flow. Laser light from the wrist-worn device shines into tissue and is then scattered back to a camera, or detector. The result is a characteristic laser speckle pattern that forms when the light interacts with blood cells passing through the patient’s circulatory system.
“The pattern produced changes over time and the rate at which it changes is directly related to blood flow,†explains Francesca Bonetta-Misteli, the lead author of a study in Biomedical Optics Express describing the new device. “We can capture these changes on video and then apply an algorithm that generates a single value per frame of video that directly correlates with blood flow.â€
The researchers initially tested their device by placing it on a tissue-mimicking platform with a hollow channel containing a milk-like liquid. When they modified the flow rate of this blood-simulating liquid, they observed a nearly perfect linear response to changes in flow. Importantly, they found that the signal measured from the device, known as the laser speckle flow index (LSFI), was more strongly correlated with the amount of blood loss than standard vital signs such as blood oxygenation levels. Further tests in live, sedated pigs undergoing blood loss produced similarly promising data.
“This result indicates that the device can accurately monitor changes in perfusion in the wrist occurring as a result of blood loss in vivo,†O’Brien tells Physics World. “What is more, the device out-performed the vital sign metrics that are the current standard for haemorrhage detection postpartum.â€
“Immense clinical applicationsâ€
The work is the first step in the development and proof-of-concept testing of the initial device prototype, she adds. “The technology has immense clinical applications as a blood flow monitor in any setting (hospital, birthing centre or rural setting). Labouring patients can wear the device during delivery and postpartum to continuously measure changes in blood flow and detect both internal and external bleeds.â€
Beyond haemorrhage, the technology could also be used to monitor the effect of medication on haemodynamics or to study cardiovascular health, she adds.

Brain bleed detection study wins AAPM’s MedPhys Slam
The Washington University team is now working to improve the design of the device (making it smaller, for example) and to develop methods for calibrating the LSFI, which would make readings more comparable between different test subjects. The researchers would also like to increase the device’s battery life and add other sensors that would give a more comprehensive picture of a patient’s condition.
“We plan to perform the same measurements with nonpregnant and pregnant patients too to study the known haemodynamic changes that occur during pregnancy,†says O’Brien. “We also want to monitor peripheral blood flow in patients who are delivering both vaginally and by caesarean to confirm that the device is able to detect postpartum haemorrhage in both cases in humans.â€




